(This article used chatGPT to organize the points and clarify them)
I. MOTIVATION: WHY WAS THIS STUDY DONE?
- Who funded the study?
- Follow the money. Industry-funded studies are significantly more likely to reach favorable conclusions.
- Ask: Would the funder lose money or credibility if the study reached a different result?
- Do the authors or institutions have any conflicts of interest?
- Look for financial ties to corporations, pharmaceutical companies, biotech firms, lobbying groups, or government contracts.
- Repeated publication history in a specific outcome direction is also a sign of narrative alignment.
- What is the stated goal of the study—and what is the real goal?
- Is the stated objective genuine scientific inquiry, or is it subtly designed to defend a product, policy, or institutional decision?
- Does the study aim to discover something new, or protect what is already assumed?
- What alternative hypothesis is being denied space?
- What competing theories, concerns, or explanations are left unmentioned?
- Ask: What isn’t being tested, and why not? Sometimes what is not studied is more revealing than what is.
II. DESIGN: HOW WAS THE STUDY BUILT?
- What was the study type?
- Randomized controlled trial (RCT)? Observational? Retrospective? Meta-analysis?
- Each design has its own blind spots. RCTs may still be biased through design choices. Observational studies may suffer confounding. Meta-analyses can be gamed by selective inclusion.
- Is it an efficacy study or a real-world effectiveness study?
- Efficacy = ideal lab conditions.
- Effectiveness = actual performance in real populations.
- Many products pass efficacy tests but fail real-world tests.
- Was there a control group—and was it valid?
- If “placebo” was used, was it truly inert? (Many “placebos” contain adjuvants or biologically active components.)
- If observational, were controls matched properly (age, sex, socioeconomic status, comorbidities)?
- Was blinding used, and who was blinded?
- Were both participants and researchers unaware of the group assignments?
- No blinding opens the door to expectation bias, consciously or not.
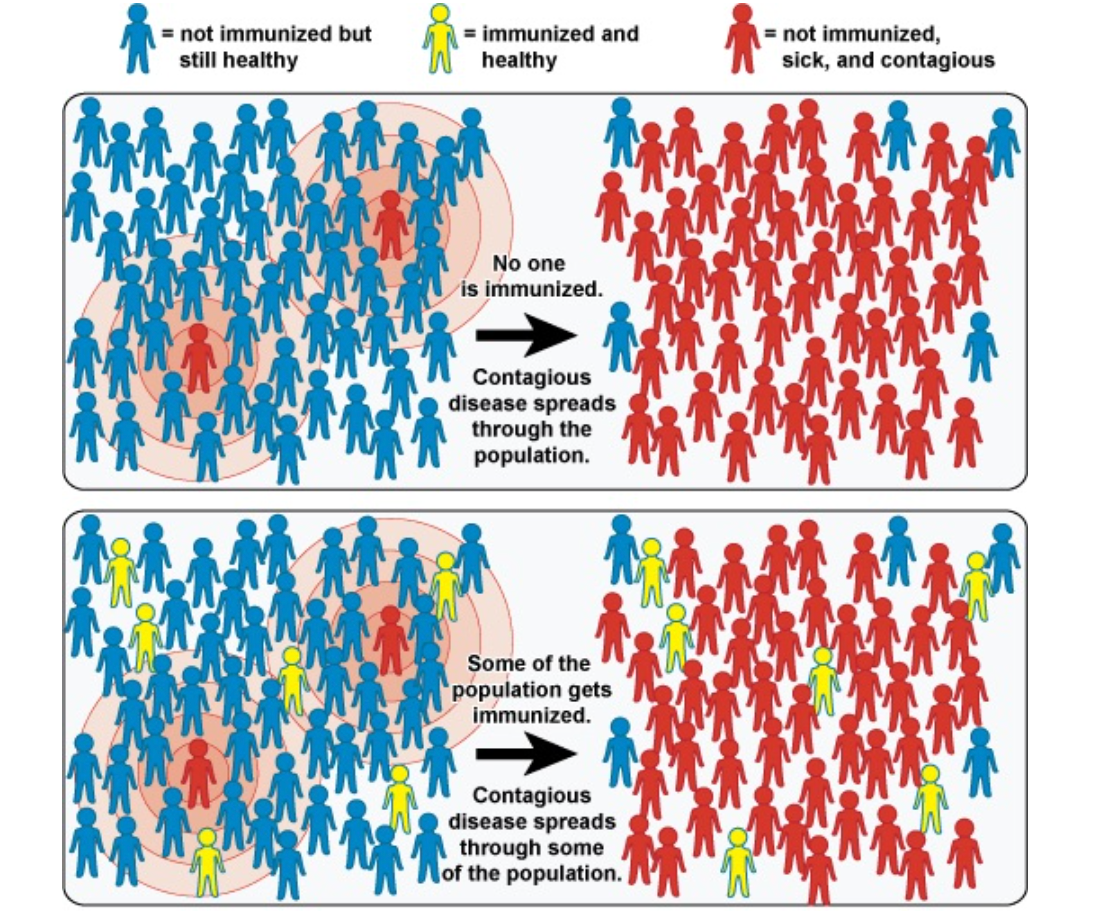
- Was the sample size large enough and relevant to the real world?
- A small study may miss real effects; an overly large one may detect meaningless “statistical” significance.
- Most importantly: Was the population representative of who will receive or be affected by the intervention?
- Was convenience sampling used?
- Were participants chosen because they were easy to recruit (e.g., students, soldiers, hospital employees)?
- Such samples are often healthier, more compliant, and not representative of general populations.
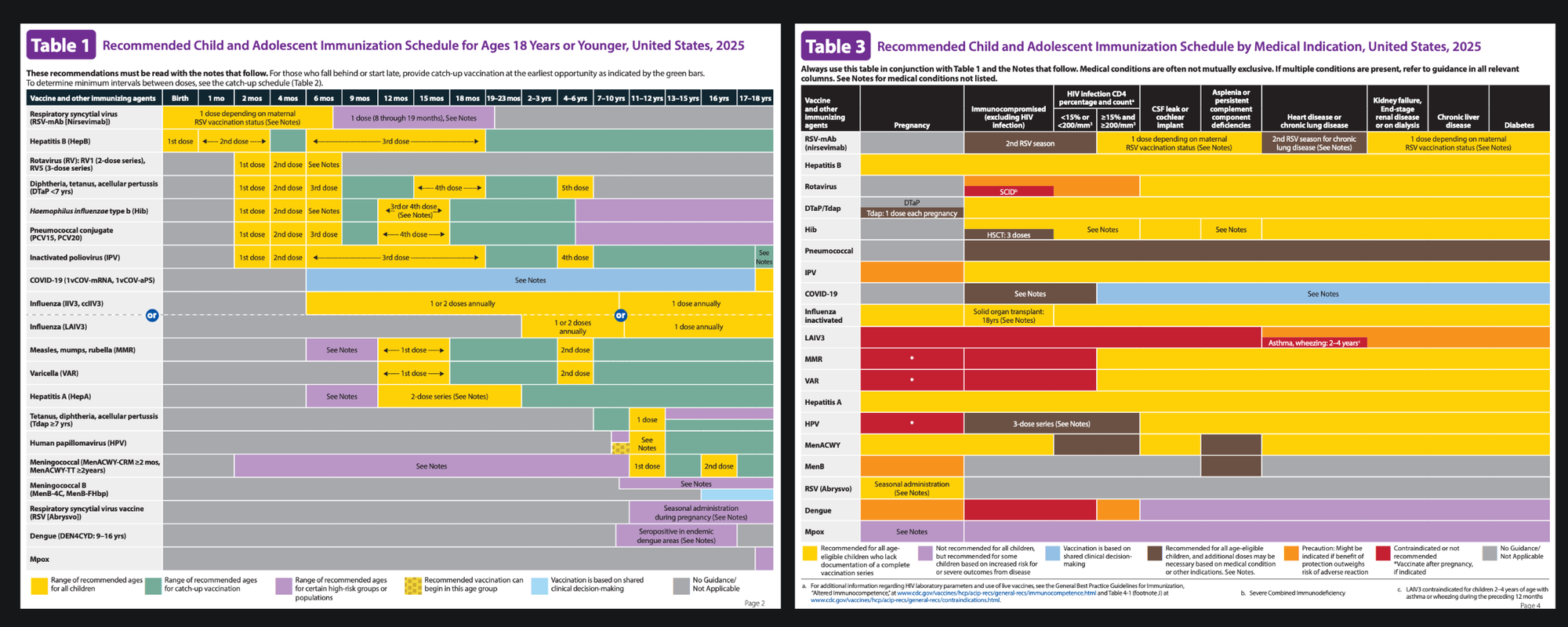
- Were any groups systematically excluded?
- Were elderly, chronically ill, pregnant, immunocompromised, or previously exposed individuals excluded?
- If so, the safety or efficacy claims do not apply to those groups.
- Were the endpoints relevant to human outcomes?
- Are the endpoints actual measures of health (survival, disease reversal), or proxies (antibodies, lab values)?
- “Increased antibodies” ≠ protection unless real-world benefit is proven.
- How long was the follow-up period?
- Was the duration long enough to observe delayed effects (e.g., cancer, autoimmune, neurological disorders)?
- Many adverse outcomes are missed simply because studies stop too early.
- What outcomes were not measured?
- Were all-cause mortality, hospitalization, and quality of life included?
- Or were inconvenient outcomes left out?
III. STATISTICS: HOW WAS THE DATA HANDLED?
- Was the study powered to detect meaningful effects?
- Did they calculate the required sample size to detect realistic differences?
- Were results presented in relative or absolute terms?
- “95% effective” may mean reducing risk from 1% to 0.05% (an absolute difference of 0.95%).
- Always demand absolute risk reductions to understand real-world impact.
- Were statistical adjustments used—and how many?
- Multivariable adjustment can control for confounding, but it can also obscure real signals.
- Excessive adjustment = data sculpting.
- Were any data excluded as “outliers”?
- Was there transparency in how and why data were removed?
- Sometimes negative results are dismissed under the guise of noise.
- Were subgroup analyses conducted—and were they cherry-picked?
- Looking at 20 subgroups guarantees “significance” in at least one due to chance.
- If no correction for multiple comparisons was applied, it's statistical sleight-of-hand.
IV. LANGUAGE AND FRAMING: WHAT WORDS ARE BEING USED?
- Is framing by negation used?
- “No evidence of harm” ≠ “evidence of no harm.”
- Such language implies safety when the study may have been underpowered or misdesigned to detect harm.
- Are minimization terms present?
- “Mild,” “transient,” “no significant increase,” “reassuring,” “well-tolerated” — these are subjective qualifiers used to downplay signals.
- Read past them and look at the raw numbers.
- Do the conclusions overreach the data?
- Are the authors making claims beyond what their data support?
- Example: A short-term antibody study concluding “long-term protection” or “safe in pregnancy” without testing either.
- Does the abstract match the body?
- Often, the abstract spins a positive interpretation, while the body shows mixed or negative data.
- Don’t rely on abstracts. Read the entire study.
- Is language used to pathologize concern?
- Watch for labeling of critics or adverse effect reports as “hesitancy,” “misinformation,” or “anti-science,” instead of addressing their arguments directly.
V. PSYCHOLOGICAL AND SYSTEMIC CONTEXT: WHY THIS MATTERS
- Is the study replicable—and has it been replicated?
- One result means little. Have others found the same?
- If replications are missing or contradictory, the original is not robust.
- Is the journal independent or industry-tied?
- Some journals have editorial boards stacked with industry consultants.
- Look for patterns of selective publication, rapid approval, or ghostwriting.
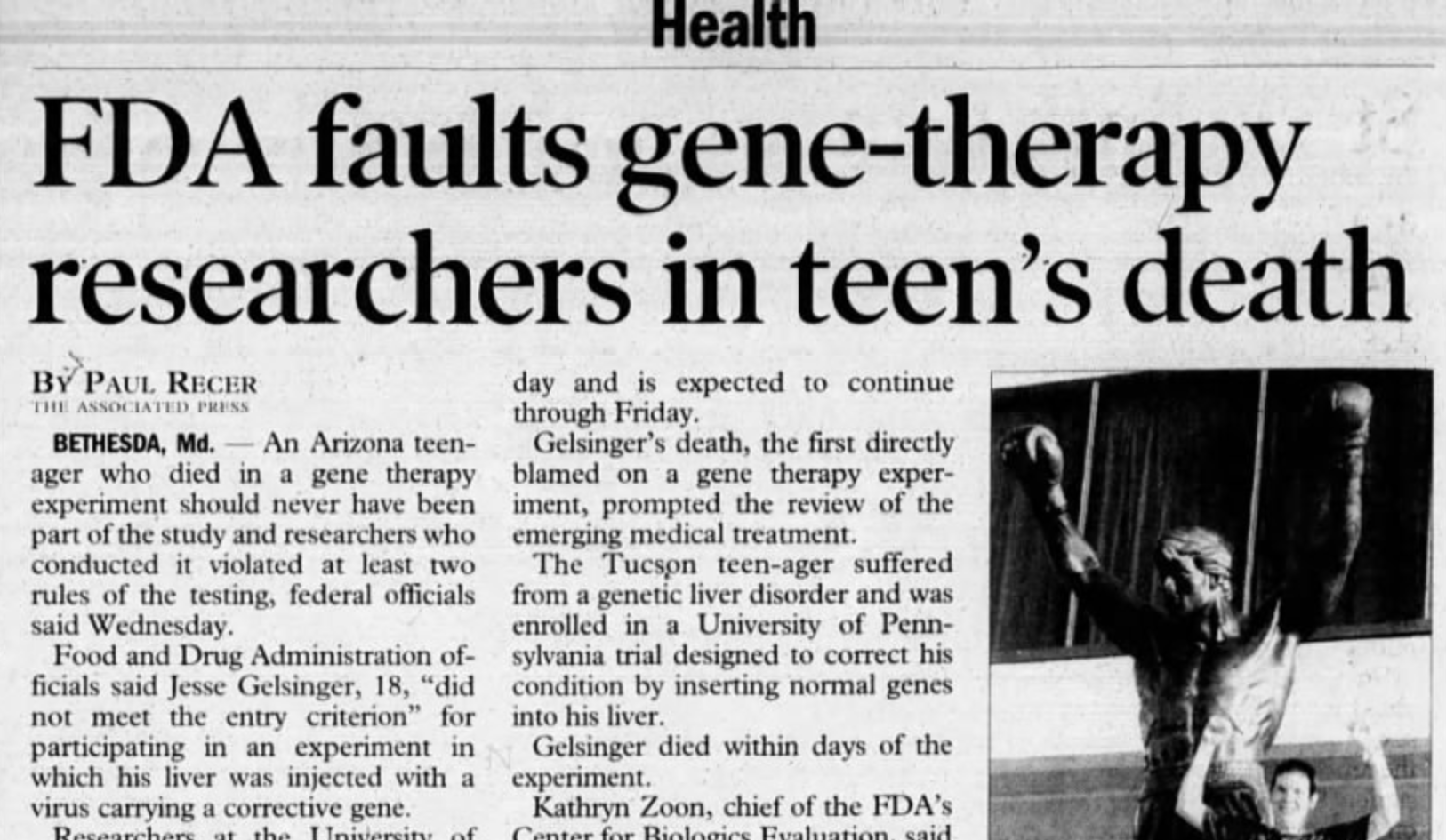
- Were adverse events transparently reported—or buried?
- Were serious outcomes disaggregated, or hidden in broad categories (e.g., “neurological event”)?
- Were outcomes clearly defined, or ambiguous?
- Was all raw data made available for independent review?
- If not, ask why. Transparency is the bedrock of science.
- Secrecy = control = possible fraud or selective omission.
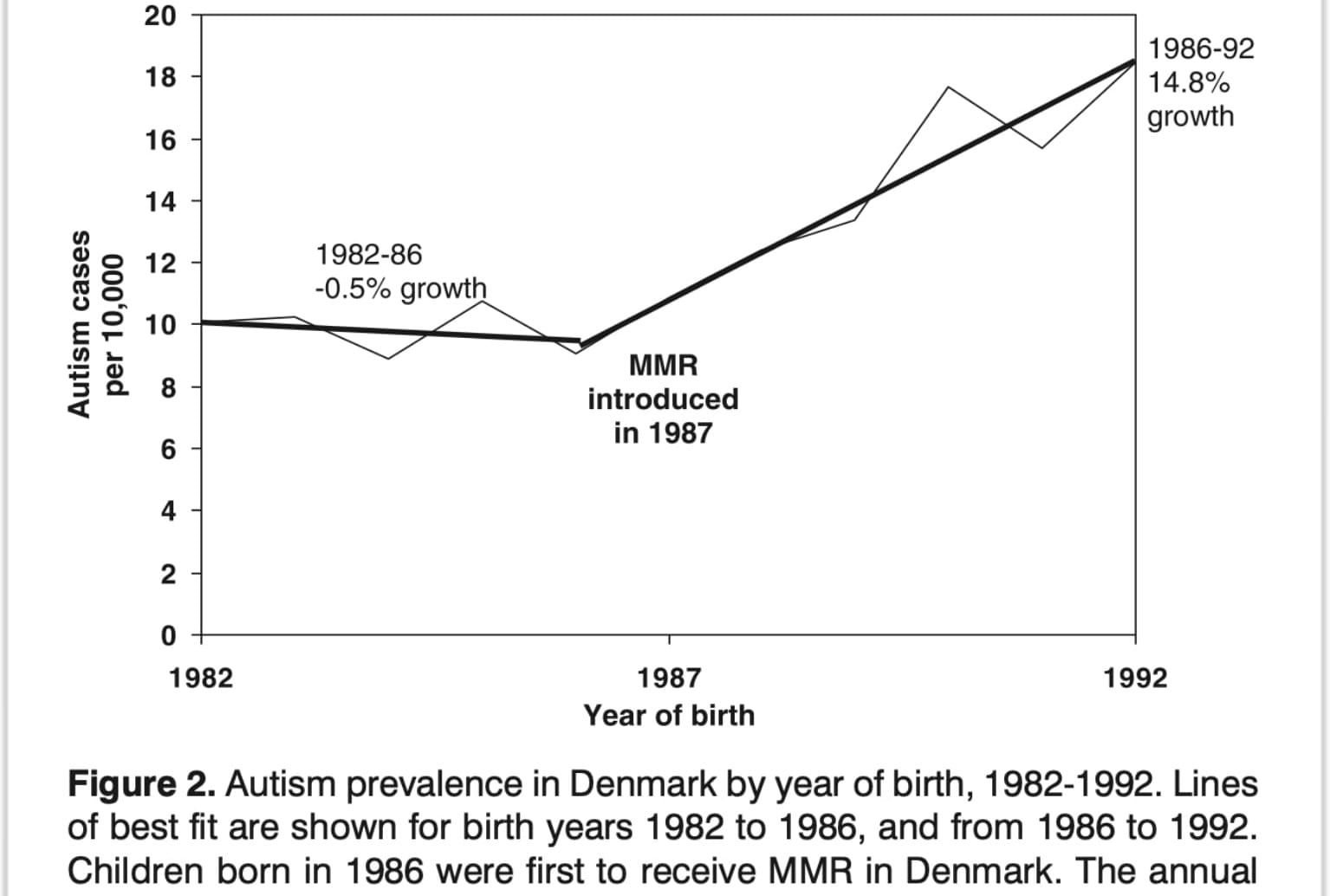
- Were relevant external data ignored?
- Did the study address or cite contradictory findings?
- If there are known adverse signals from real-world surveillance, and these are unmentioned, it signals narrative protection.
- Who benefits if the conclusion is accepted?
- Is there a policy, product, mandate, or narrative that this study upholds?
- Understanding the power structure behind the science is essential for interpretation.
Final Principle: Science ≠ Neutral
Every study is a story told by humans, often within institutions that have agendas, liabilities, markets, and fears. This guide does not mean rejecting all science—it means learning to read it as a system of persuasion as much as a system of discovery.
The question is not just "What does the study say?"
But always: "What does it allow itself to say—and what does it silence?"
Use this framework every time. It applies across disciplines, whether you're reading about a new drug, food additive, medical device, behavioral program, or environmental policy.
This is not skepticism.
This is literacy.




Discussion